Spine Disorders, Diseases & Deformities
Spinal Conditions
Neurosurgical spine care at Advanced Neurosurgery Associates (ANA) focuses on all types of back, neck, spine, and spine-related disorders, from common spine problems to the most complex spinal disorders. Our surgical solutions address everything from spine diseases to conditions that cause recurring and often life-altering pain.
Common Spine Problems
Back pain is ranked second only to headaches as the most frequent cause of pain among Americans. Up to 80 percent of the population experiences a bout of back pain at some time in their lives.
Fortunately, the vast majority recover from spinal issues with no medical or surgical intervention. However, for others, back problems can interfere with everyday life.
Complex Spine Disorders and Diseases
Spinal injuries and diseases are among the most complex ailments encountered in medical practice.
Many of our patients suffer from a broad range of disease processes that can affect the spine, including:
- degenerative conditions such as lumbar and cervical disc diseases and rheumatoid arthritis
- compression syndromes
- spinal cord and vertebral tumors
- spinal cord malformations
- spinal trauma and infections.
Causes of Spine Issues and Conditions
Spinal issues can result from a range of causes, including:
- disease
- abnormal development from birth (congenital)
- from aging or “wear and tear” (degenerative)
- trauma from an injury, from infection from a tumor (neoplastic)
- related to other medical conditions.
At ANA, we are experienced in a complete range of services for the diagnosis, treatment and rehabilitation of patients with spine and peripheral nerve disorders.
Symptoms of a Spine Disorder
Signs of a spine disorder or disease vary depending on the location and type of the spine condition. It is not uncommon for a severe spine issue to cause problems in other parts of the body.
Some symptoms to look for include:
- pain in your back or neck that feels like a dull ache, burn, sharp stabbing, stiffness or tightness.
- nausea or vomiting
- unusual sensations in the arms or legs, such as radiating pain, weakness, numbness, or tingling
- excessively rounded shoulders or a crooked spine
- uneven shoulders or hip bones
- issues with the bladder or bowel.
Our expertise includes neurosurgical evaluation and surgical solutions for:
- neck and back pain
- herniated intervertebral discs
- nerve and spinal cord compression syndromes.
Neurosurgeons were among the first experts to operate on the spine, and their experience has resulted in the evolution of spinal surgery. At ANA, we believe that our training and experience in handling the delicate issues of the brain enhances our ability to effectively perform surgery on the spine and the nerves that are involved.
Read our guide on Back and Neck Pain for more information.
Anatomy of the Spine
It is helpful to have a basic understanding of the anatomy and function of the spine to better understand how problems arise.
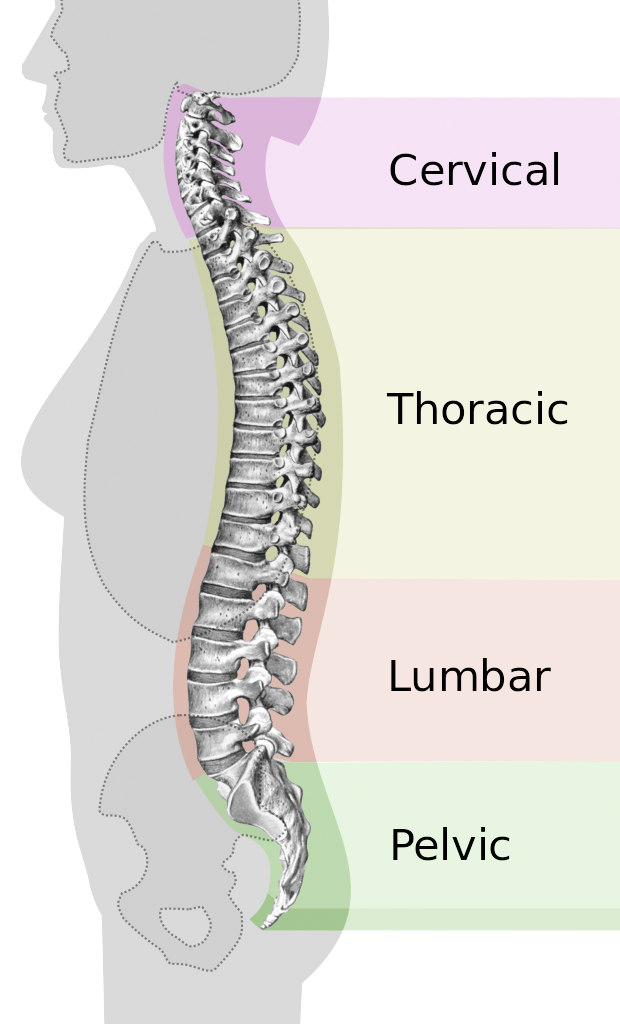 The spinal column is made up of 33 vertebrae that are separated by spongy discs. The spine is divided into distinct areas: cervical, thoracic, lumbar and sacral. Ligaments and muscles connect the bones together and keep them aligned.
The spinal column is made up of 33 vertebrae that are separated by spongy discs. The spine is divided into distinct areas: cervical, thoracic, lumbar and sacral. Ligaments and muscles connect the bones together and keep them aligned.
The spinal column provides the main support for the body, allowing a person to stand upright, bend, and twist. The many muscles that connect to the spine help support the upright posture and movement of the spine.
The normal spine has an “S”-like curve when looking at it from the side. This allows for an even distribution of weight. The “S” curve helps a healthy spine withstand all types of stress.
The spinal, or vertebral, column holds and protects the spinal cord, which is a bundle of nerves that sends signals to other parts of the body. The spinal cord is a major part of the central nervous system. It carries sensory and movement signals to and from the brain and controls many reflexes.
The spine reaches from the base of the skull to the coccyx (tail bone). The bones of the spine and a sac containing cerebrospinal fluid surround the spinal cord.
For more information about our Neuro-Spine Center, its specialists and any additional questions you may have please contact us at: (201) 457-0044.